Prolapse

What is a prolapse and why do they happen.
A prolapse occurs when one or more of the organs in the pelvis shift from from their normal position and push on the walls of the vagina, or in the case of the uterus, bulge into into.
There are four main types which involve the womb (uterus), bowel, bladder or top of the vagina.
A prolapse can cause pain and discomfort but it is not life threatening.
In many cases symptoms can be improved with pelvic floor exercises and lifestyle changes, but in some cases medical treatment may be required.
What are the symptoms of a prolapse?
Symptoms include:
- a feeling of heaviness around your pelvis and/or genitals
- a sensation of ‘dragging’ or ‘weight’ inside your vagina
- feeling like there’s pressure or something coming down into your vagina – it may feel like sitting on a small ball
- feeling or seeing a bulge or lump in or coming out of your vagina
- pain or numbness during sex
- problems urinating or poohing– including feeling like your bladder or rectum is not emptying fully, needing to go to the toilet more often, or leaking a small amount of pee when you cough, sneeze or exercise (stress incontinence)
Sometimes, however, there are no symptoms and it is found during an internal examination such as cervical screening.
If you have any of these symptoms or if you notice a lump in or around your vagina make an appointment to see your GP who may, with your permission, do an examination or refer you to a gynaecologist or for further tests. (Remember you can ask for a female doctor or for a chaperone to be present during the examination.)
What causes a prolapse?
Our pelvic organs are held in place by the group of muscles and ligaments that for the pelvic floor. If they become weak the organs can slip from their normal position and affect the other nearby organs – usually the vagina.
Things that can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse include:
- pregnancy, childbirth or trauma during childbirth
- ageing
- declining oestrogen levels associated with menopause
- being overweight
- having long-term constipation
- a long-term health condition that causes you to cough which puts strain on the pelvic floor
- having had a hysterectomy
- frequent heavy lifting
- previous pelvic floor surgery
Other health conditions can increase the risk of a prolapse include:
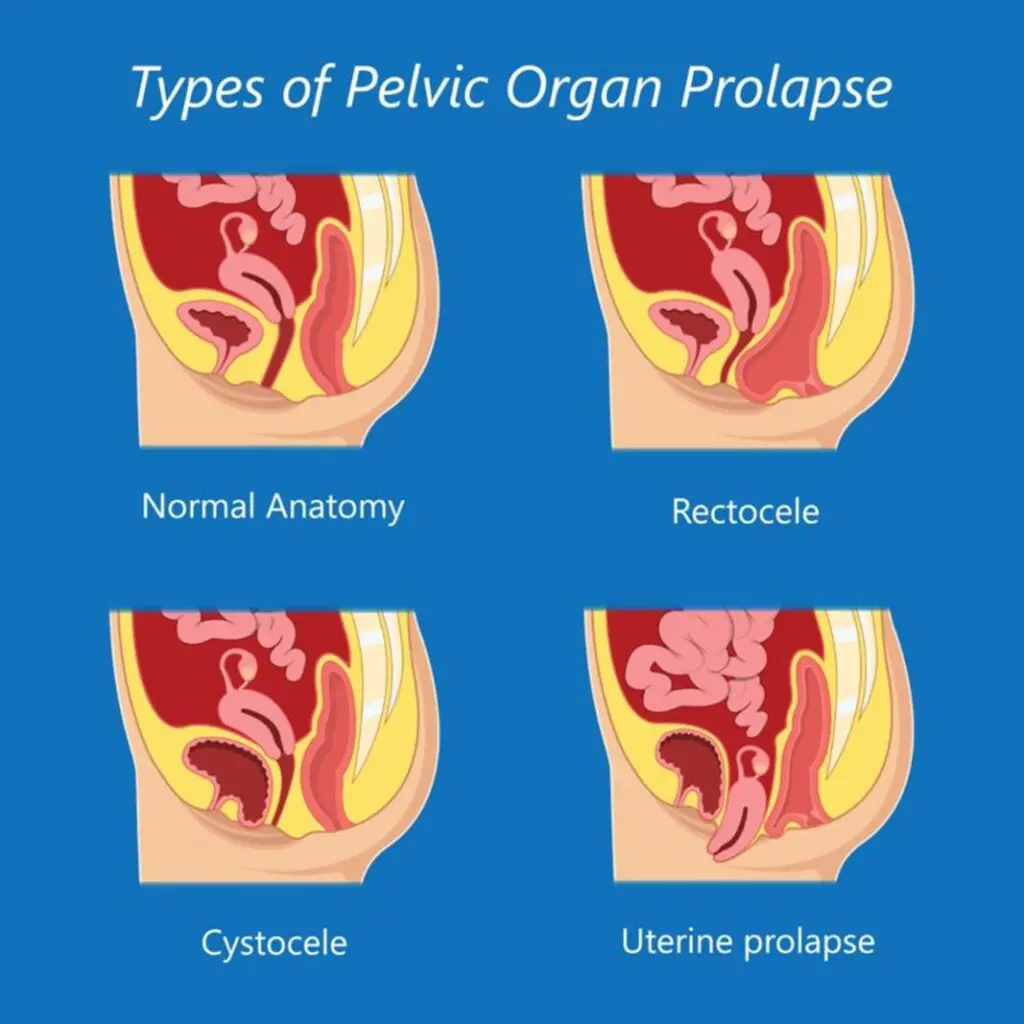
What are the types of prolapse?
There are 4 main types of prolapse:
- the bladder bulging into the front wall of the vagina (anterior prolapse or cystocele)
- the womb bulging or hanging down into the vagina (uterine prolapse)
- the top of the vagina sagging down – this sometimes happens after surgery to remove their womb
- the bowel bulging forward into the back wall of the vagina (posterior wall prolapse – rectocele)
Sometimes more than one of these is involved.
Prolapses are classified on a scale of 1 to 4 with 4 being the most severe.
A woman with a grade 1 prolapse may not notice she even has an issue until it is picked up in a routine smear test.
How do you treat a prolapse?
If you do not have any symptoms, or the prolapse is mild and not bothering you, some lifestyle changes could help improve it, and possibly prevent it from getting worse.
These include:
- losing weight if you’re overweight
- avoiding heavy lifting or adopting good lifting techniques
- preventing or treating constipation.
(Tip: A squatty potty! Find a small foot stool or something you can use in the toilet to put your feet on when you go to the loo. It should raise your knees above the height of your hips – and this changes the angle of the pelvis and the pooh passed out more easily.)
If the prolapse is more severe or your symptoms are affecting your daily life, there are several further treatment options to consider.
These include:
- pelvic floor exercises
- hormone treatment
- vaginal pessaries
- surgery
There are many different types of pessary but most are inserted into the vagina and are used to help support the cervix or neighbouring bladder or rectum.

The recommended treatment will depend on the type and severity of the prolapse, your symptoms, you age and your overall health, and whether or not you are planning in having children in the future.
Your doctor discuss the the full range of treatments with you and explain the possible benefits and risks of each option. This will help you choose the right one for you.
1. Lifestyle changes
A good set of lifestyle habits can help prevent a prolapse or improve symptoms if you have one.
They include:
- losing weight if you’re overweight
- eating a high-fibre diet to avoid constipation
- avoiding lifting heavy objects or ensuring you have a good lifting technique.
2. Pelvic floor exercises
Pelvic floor exercises can help strengthen your pelvic floor muscles and may well relieve your symptoms.
Your doctor may recommend a 16 week supervised pelvic floor muscle training programme before you move on to other treatments or surgery. There are apps that can help with this too, such as the Squeezy App.
A good pelvic floor physiotherapist can help too.
Please remember that there is more to a pelvic floor exercise than simply squeezing – they need to be done correctly and they are not suitable for everyone.
Tip: there are many ‘weights’ for the vagina – but before you buy them, check with your practitioner about their suitability. Also, never out porous stones like jade into your vagina as they can harbour bacteria and increase your risk of infection.
3. Hormone (oestrogen) treatment
If you have a mild prolapse and have been through the menopause or are breastfeeding, your doctor may recommend treatment with a topical oestrogen to ease some of your symptoms, such as vaginal dryness or discomfort during sex.
Topical oestrogen is available as:
- a cream you apply to your vagina
- a tablet you insert into your vagina
- an oestrogen-releasing vaginal ring
4. Vaginal pessaries
These are devices made from rubber (latex) or silicone which are inserted into the vagina and left in place to support the vaginal walls and pelvic organs.
You can have sex and you can still get pregnant. They can be used to ease the symptoms of moderate or severe prolapses and are a good option if you can’t or would prefer not to have surgery.
They come in different shapes and sizes depending on your need. The most common is called a ring pessary.
You may need to try a few different types and sizes to find the one that works best for you.
A gynaecologist or a specialist nurse usually fits a pessary. It needs to be removed, cleaned and replaced regularly.
Side effects?
Vaginal pessaries can sometimes cause:
- an unpleasant smelling vaginal discharge, which could be a sign of an infection knowns as bacterial vaginosis
- irritation or sores inside your vagina which may bleed
- stress incontinence, where you pass a small amount of urine when you cough, sneeze or exercise
- a urinary tract infection
- interference with sex (but this is uncommon)
Prevention
To reduce your risk of uterine prolapse, try to:
- Perform Kegel exercises regularly to strengthen the pelvic floow if they are appropriate for you you. These exercises are especially important after you have a baby.
- Treat and prevent constipation. Drink plenty of water, and eat high-fibre foods, such as fruits, vegetables, beans and whole-grain cereals. Avoid too much caffeine and alcohol. Exercise regulalry.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough, and try to quit smoking.
- Avoid weight gain. Talk with your doctor for advice on weight-loss strategies, if you need them.
Surgery
If non-surgical options have not worked or the prolapse is more severe, surgery may be an option.
There are several different surgical treatments for pelvic organ prolapse.
They include:
- surgical repair
- hysterectomy
- closing the vagina
1. Surgical repair
There are several different types of surgery that involve lifting and supporting the pelvic organs. They may be stitched into place or it could involve supporting the existing tissues to make them stronger.
Surgical repairs are done under general anaesthetic and done via cuts made in the wall of the vagina.
You may need 6 to 12 weeks of recovery.
If you’re planning on having children in the future your doctor may suggest delaying surgery because pregnancy can cause the prolapse to happen again.
2. Vaginal mesh surgery
It’s not possible to have vaginal mesh surgery for prolapses on the NHS unless there’s no alternative and the procedure cannot be delayed. It is not performed now unless there is no other choice as a number of women had serious complications after mesh surgery.
It surgery involves the insertion of synthetic mesh, a plastic product that looks like a net, to hold the pelvic organs in place.
The mesh stays in your body permanently. Some, but not all, of these complications can also happen after other types of surgery.
The complications include:
- long-lasting pain
- permanent nerve damage
- incontinence
- constipation
- sexual problems
- mesh exposure through vaginal tissues and occasionally injury to nearby organs, such as the bladder or bowel
If you have had vaginal mesh inserted and think you’re having complications, speak to a GP or your surgeon.
If you’re not having any complications, there’s no need to do anything.
You can report a problem with a medicine or medical device on GOV.UK.
3. Hysterectomy
A hysterectomy may be suitable for women with a prolapsed womb who have been through the menopause or do not wish to have any or any more children. You can read more about hysterectomies here.
It is used to help to relieve pressure on the walls of the vagina and reduce the chance of a prolapse returning.
You cannot get pregnant after having a hysterectomy, and sometimes it may cause you to go through the menopause early. Again, you may need 6 to 12 weeks off work to recover.
4. Closing the vagina
Occasionally, an operation that closes part or all the vagina may be an option for women who have advanced prolapse, when other treatments have not worked and they’re sure they do not plan to have sexual intercourse again in the future.
This operation may be suitable for frail women who would not be able to tolerate more complex surgery.
Side effects of surgery
Before you undertake surgery you should be informed by your doctor about all your options and the risks and benefits associated with each.
You should decide together which is most appropriate for you and you are entitled to seek a second opinion.
Your surgeon must keep detailed records about the type of surgery they do and any complications you may have after surgery. You should be given a copy of this record.
All Possible side effects of all 4 types of surgery include:
- risks associated with anaesthesia
- bleeding, which may require a blood transfusion
- damage to the surrounding organs, such as your bladder or bowel
- an infection – you may be given antibiotics to take during and after surgery to reduce the risk
- changes to your sex life, such as discomfort during intercourse – but this should improve over time
- vaginal discharge and bleeding
- experiencing more prolapse symptoms, which may require further surgery
- a blood clot (DVT) forming in 1 of your veins, such as in your leg – you may be given medicine to help reduce this risk after surgery
You should be offered a check-up 6 months after surgery which includes a vaginal examination.
More information to help you choose which type of prolapse surgery
There are 2 useful guides that you can read to help you decide, together with your doctor, which type of surgery would be right for you:
- Surgery for pelvic organ prolapse decision aid (PDF, 662kb)
- NHS guide to surgical treatments for pelvic organ prolapse
Sources: NHS, Mayo Clinic

