Menopause symptoms

Do your Menopause Symptoms Really Fade Away After Menopause?
There’s a perception that menopause symptoms fade away within several years of your periods stopping and post-menopausal life goes blissfully on, but a growing body of research is challenging that.
We know that vasomotor symptoms (VMS) usually start in perimenopause and for most women last around 7.4 years[1]. They usually persist after menopause for around 4.5 years, so with an average age of menopause at around 51 years of age, you’d expect them to be done and dusted by the mid 50’s for the majority of post-menopausal people.
We also know that around 10%[2] of women aged between the age of 60-65 still experience them hot flushes and night sweats and what’s generally termed ‘a handful’ of people may continue to have them into their 80’s.
But the recently published “2023 Practitioner’s Toolkit for Managing Menopause”[3] suggests the number of women with persistent vasomotor symptoms is significantly higher. It cites studies saying 42% of 60–64 years and 33% of women aged 65–79 years were still having moderate to severe vasomotor symptoms and the authors noted that these symptoms can severely impact both physical and mental health.
The study says women with moderate-to-severe vasomotor symptoms are up to three times more likely to have moderate–severe depressive symptoms than other women and were also likely to experience other menopause-associated symptoms include anxiety, disturbed sleep, joint pain, vaginal dryness as well as urogenital symptoms such as continence issues and more frequent urinary tract infections (UTIs). Untreated moderate-to-severe vasomotor symptoms have also been associated with an increased risk of heart attacks and stroke[4].
And contrary to commonly held beliefs that these symptoms were a phenomenon of western society it cited studies from Japan[5], Bangladesh[6] and Iran[7] showing similar findings.
“These symptoms, when due to estrogen deficiency, persist unless treated, and potentially all untreated postmenopausal women are affected,” the authors wrote.
Quote: “Thought I was doing OK! Worst symptoms post menopause!”
Harley Street Emporium has conducted a survey of UK based women aged 55 or over to see which symptoms are of most concern to them, and the list is long. Data from the second phase of analysis of 110 de-identified respondents who answered the survey on the website shows that 50% of women aged 55-75 were still experiences hot flushes and night sweats. Of those, 30% said hot flushes were their main concern while 40% said night sweats were their main issue, and 30% said both were an issue.
But these weren’t the only concerns the 110 respondents listed.
Poor sleep affected 79%, followed closely by brain fog at 71%. Low libido came in just behind that at 68% with low mood and anxiety effecting 60% of respondents.
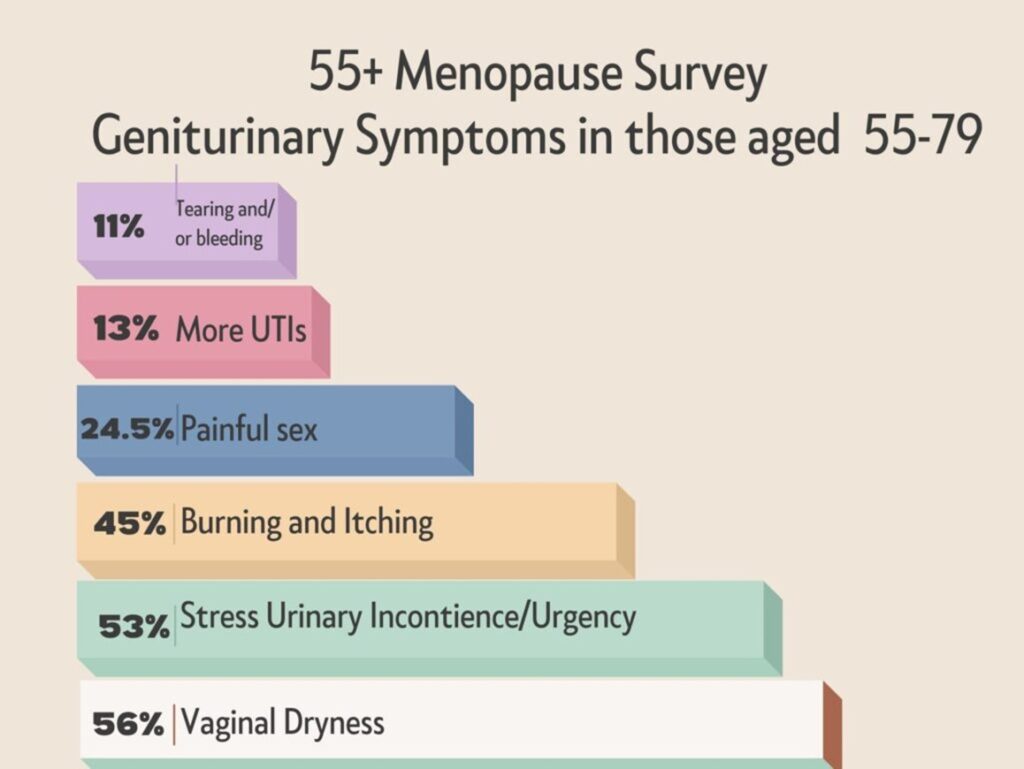
It’s sometimes estimated that as much as 70-90% of post menopausal women will have genitourinary symptoms and only 7% will get them treated. This survey showed 56% said they had vaginal dryness which is in line with other estimates[8]. Another study[9] of 1548 women aged 65-70 showed that 32.5% of this group experienced vaginal dryness.
Quote: “Menopause took my marriage, career and almost my sanity.”
When it came to bladder issues like stress urinary incontinence (leakage) and urgency (the need to go ‘right now’) 53% said they were a concern.
Itching and burning affected 45%, painful sex was an issue for 24.5% and an increased frequency of urinary tract infections affected around 13% of respondents.
Interestingly, we say the average age of menopause is 51 with a range of 45-55, but 33% of the survey respondents over the age of 55 said they were still having periods or perimenopausal. And those who were still having periods seemed to experience less of the symptoms than those who were post menopausal.
Do the symptoms fade away?
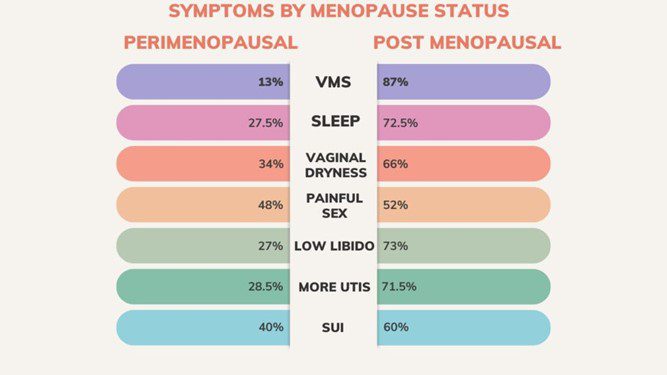
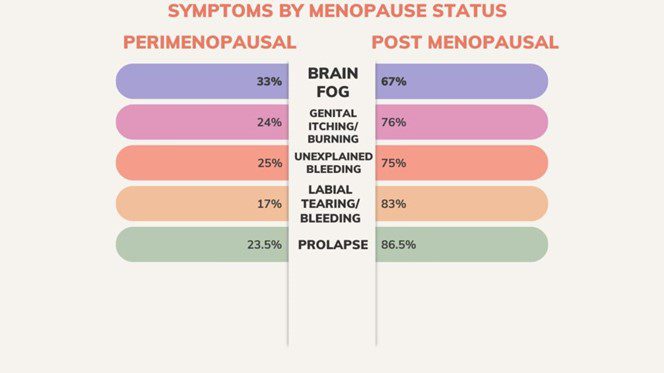
We tend to focus on symptoms in perimenopause but for every symptom in this survey the post menopausal women experienced them more often than their perimenopausal counterparts. The only exception was bacterial vaginosis (BV) where it was equally split between the two groups.
The study is limited in that the number of perimenopausal women in this group was around a third, but the results show that the symptoms aren’t fading away in those who are post menopause with 87% of post menopausal people saying they were experiencing vasomotor symptoms as opposed to 13% of those who stated they were perimenopausal. Poor sleep, low libido an and increase in the frequency of UTIs effected double the number of post menopausal people than their perimenopausal counterparts. Painful sex was about equal in bot groups.
When it came to sexual activity just over a quarter of participants had had sex within the last 7 days, but a staggering 80% of them said sex was ‘too painful’.
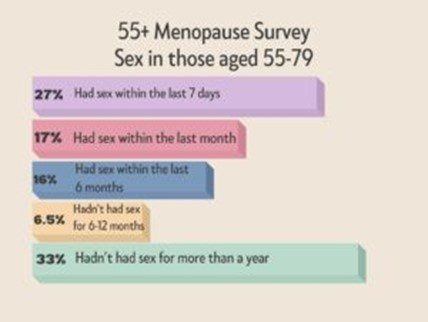
Some 53% of respondents said sex was ‘too painful’ and one third said they hadn’t had sex for more than a year.
Other reasons given for not having sex were ‘no interest’ (23%), while 11% ‘chose not to’ and an equal number said they had ‘no partner’.
Fact:
80% of women over 55 who’ve had sex in the last 7 days said it was ‘too painful’.
When it came to seeking help respondents were almost equally split with satisfaction levels. Some 39% said they were either very dissatisfied or dissatisfied with the help they received while 44% said they were satisfied or very satisfied.
Quote: “I suffered hugely as I didn’t know about it. Low mood and anxiety and had quite a struggle to get HRT.”
Interestingly, while NHS GPs in particular appear to bear the brunt of dissatisfaction from people seeking help for their symptoms, 37% of respondents said they were satisfied or very satisfied.
Unfortunately 42% felt the other way saying they were dissatisfied or very dissatisfied.
Private GPs scored better with 66% saying they were satisfied, but online providers were not popular with 66% saying they were very dissatisfied with the service they recieved.
People were split over the care the received at hospital gynaecology/menopause facilities with 45% saying they were happy and an equal number saying they weren’t, while 10% said they were neither satisfied nor dissatisfied.
Specialist menopause clinics scored better with 60% of respondents saying they were satisfied or very satisfied and 20% saying they were dissatisfied or very dissatisfied.
About one third of respondents (34%) said it was difficult or very difficult to get access to their GP, 30% said it was neither easy/nor difficult and 25% said it was easy or very easy.
Just over a third of respondents (36%) had other conditions that affect their gynaecological health. Fibroids and prolapses were the most common, affecting 10% respectively. Gynaecological cancers affected 3% and an equal number had endometriosis or polyps.
Support at home and at work
At work just 37% of respondents said they felt supported or very well supported, not no one said they felt very unsupported. And when it came to support outside of the work place:
- 22% said they had no support
- 46% said they relied on their partners or family members
- 22% said friends were their rock
- 4% said their doctor
- 6% said ‘other’ but didn’t specify who.
Who responded to the survey?
Of those who answered about their level of education 16% had finished school, 19% had completed technical training or an apprenticeship, 45% has an undergraduate degree and 20% had a post-graduate qualification.
Some 43% were employed, 26% were self-employed, 21% were retired and 10% were unemployed.
Two respondents identified themselves as non-binary while 13 gave no answer on their gender identity. The remainder identified as female.
Quote: “I thought I had coped well to 58 but now it feels as if I am falling apart mentally and physically!”
Summary
Menopause symptoms do not stop being an issue for women over the age of 55.
The vast majority of respondents had multiple symptoms, all of which impact on quality of life, the ability to work and relationships, as reflected in the comments given. Metal health, brain for and genitourinary symptoms have a considerable impact on relationship, family and our ability to work, and with an estimated 4.5 million UK women in the work force aged between 60-65 dealing with these issues is a priority.
The extent of the symptoms across all aspects in post menopause means we need to start looking at this population differently. We need to recognise and take these symptoms seriously with appropriate information on lifestyle and medications so women can make informed choices about their future health. These are not just symptoms of aging, they’re symptoms of menopause and should be addressed as such.
Women need help and support post menopause. We are living at least one third of our lives in post menopause and it should not be spent in physical or mental pain.
References:
[1] https://pubmed.ncbi.nlm.nih.gov/25686030/#:~:text=Main%20outcomes%20and%20measures%3A%20Total,FMP%20persistence%20was%204.5%20years.
[2] https://journals.lww.com/menopausejournal/fulltext/2023/12000/prevalence_and_impact_of_vasomotor_symptoms_due_to.3.aspx
[3] Climacteric Volume 26, 2023 – Issue 6
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10377626/
[5] Akiko S, Kawaharada M. Associations between hot flashes, obesity, sense of coherence and qol among japanese farmers and part-time workers. Climacteric. 2011;14:187.
[6] https://pubmed.ncbi.nlm.nih.gov/26926325/
[7] https://pubmed.ncbi.nlm.nih.gov/30145921/
[8] https://www.racgp.org.au/afp/2017/july/genitourinary-syndrome-of-menopause#:~:text=The%20symptoms%20range%20from%20mild%2C%20moderate%20to%20
debilitating.&text=Other%20studies%20have%20found%20that,loss%20of%20oestrogen%20at%20menopause.

