Progesterone

Confused about how to use progesterone or you don’t tolerate it well? Dr Juliet Balfour explains your options.
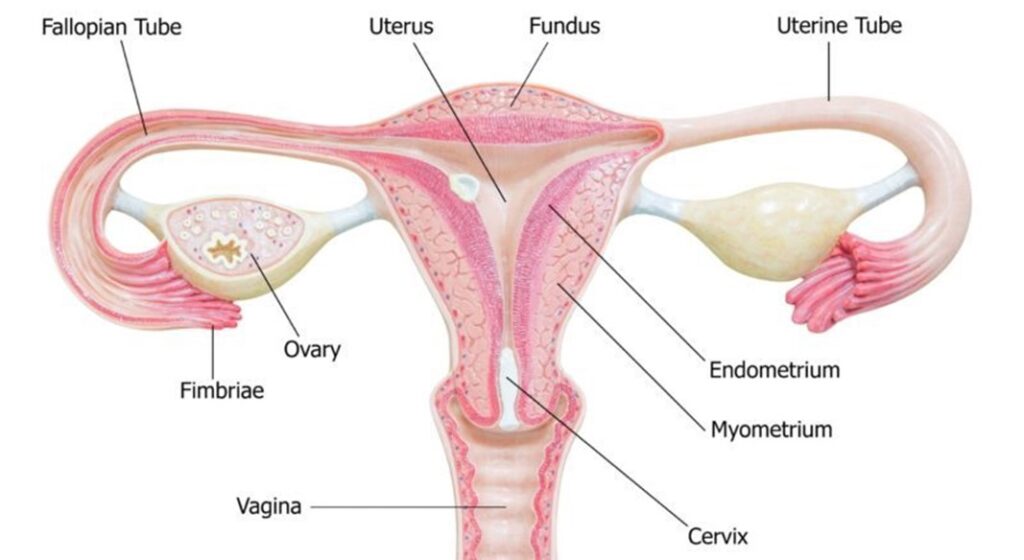
If you have a uterus you need progesterone as part of your HRT. It is vital for controlling the thickness of the endometrium or lining of the womb. By stopping it from becoming too thick it reduces our risk of endometrial or womb cancer.
Dr Juliet Balfour, a menopause GP from Somerset says progesterone is produced by our ovaries and in our fertile years its job is to prepare the womb for pregnancy. If we don’t get pregnant the levels drop and we have a period. It can be the cause of premenstrual syndrome or premenstrual dysphoric disorder (PMDD) which may be caused by an intolerance to it.
When we get to menopause we need it to protect the lining of the womb. “If you just have oestrogen the lining will gradually get thicker and may develop abnormal cells that may develop into cancer, so it’s very important to have it as part of your HRT if you still have your uterus”, Dr Balfour says.
If you had a hysterectomy do you still need it?
It would depend on what type of hysterectomy, Dr Balfour says. If your cervix is still in place then you may need it as there may be some endometrial tissue that’s been left behind, or if you have endometriosis progesterone may be required. Many women have surgery to remove the endometrial tissue but sometime some tissue may remain and progesterone will be needed to help control the symptoms.
Better Sleep?
Another group of people who may benefit from it – with or without a uterus- are people with insomnia. Some women find that progesterone helps them sleep if they take it with a bit of food a couple of hours before they go to bed.
When it comes to types of progesterone there are a number of options.
Progesterone based products like Utrogestan are “body identical” – they are made from yams and match the progesterone you would naturally make yourself.
Progestins are synthetic versions of progesterone and are used mostly in oral forms or the mirena coil which is inserted into the uterus via the vagina and sits in place for 4-5 years.
Progesterone, like Utrogestan, that is body identical does not have the same risks as the synthetic versions when it comes to blood clots.
If you are still having periods you can take 2 tablets of this for 12 or 14 days a month while using/taking your oestrogen daily. The is known as sequential HRT.
“You may bleed while you taking the progesterone or for a few days after you stop”, Dr Juliet says.
Once you’ve been taking it until around the average time that women would normally go through menopause (around 51 in the UK) you can swap to what’s called continuous combined HRT. This is where you take/use the oestrogen every day and 1 progesterone tablet every night without a break and that’s designed to give you no bleeding.
Dr Balfour says irregular bleeding can be an issue but it may settle down over time but sometimes dosages and types of HRT may need to be changed.
What is I have uncontrolled bleeding?
She says any abnormal bleeding needs to be checked by your GP. “If you haven’t had a period for a year and you start to bleed, then that needs to be checked immediately as it may be an indication that your endometrium is thickening.”
“Utrogestan is often well tolerated but may not be the best for controlling bleeding, so sometimes we try synthetic progetins that can sometimes be better”, she says.
One option is the mirena coil. It is an IUD that goes into the uterus and protects for up to 5 years. It can be used as contraception as well.
She says insertion is quick and there may be a little sharp pain but it’s over quickly and then it’s set and forget for the next 5 years. It acts locally, very little gets into the system, she says.
A Question of Tolerance
Most people tolerate it well – but there are some that find all forms of progesterone or progestins give them troubling side effects. These can include fatigue, low mood, irritability, bloating and spottiness – very similar to PMS.
“Some people just don’t get on well with it. Often people who get PMS when they’re younger struggle with it. We can try a variety of patches, tablets or the coil but there are a small number of women who just don’t get on with it. Women who found certain type of the contraceptive pill didn’t suit them often struggle” Dr Balfour says. “It’s worth struggling on with for a few months to see if it settles.”
Utrogestan is licenced to be taken orally but it can also be used vaginally – and some women may tolerate this better and she says and she adds, we know it is absorbed well. You should tell your GP that you are using it this way and please note it may affect condoms if you are using those for contraception.
You use the same dose but insert the tablets into the vagina as far as you can, Dr Balfour advises.
Another option are the combined patches such as Evorel Conti and Evorel Sequi. These have both body identical oestrogen and the synthetic progestin.
They only come in one dose but can be chopped in half if you need more or less. They come in a continuous patch with both oestrogen and progestin for every day use or the sequential which has oestrogen every day but progestin for two weeks of the cycle.
Tips for patches: make sure you’re applying them to dry skin. Do not apply moisturiser before you put the patch on.
Femiston is another oral HRT option which has a different a type of progestin, dydrogesterone, that seems to be tolerated better than other forms of synthetic progestins.
In terms of risk for blood clots and breast cancer the safest is Utrogestan. “So many people don’t realise that it’s the type of progestin/progesterone that may be associated with breast cancer, not the oestrogen.”
If you need contraception, Dr Balfour says you may also need to take the mini-pill in addition to Utrogestan.
Dr Balfour warns against the use of progesterone creams as they are unregulated and often do not absorb well.
She also says it is dangerous for women with a uterus to only take oestrogen. Women are often told they are ‘oestrogen dominant’ and she says there is no scientific evidence to back this claim.
“I’m afraid I don’t subscribe to it”, she says. “Dare I say it, it’s pseudo science.”
Tip for women with polycystic ovarian syndrome (PCOS) – make sure you are having a bleed at least 4 times a year. Discuss a regime that would ensure this with your GP to ensure your endometrium isn’t becomg too thick.Watch the full interview with Dr Balfour here: https://www.instagram.com/tv/COBJkpzlBX6/?utm_source=ig_web_copy_link

