Pelvic floor health

From prolapses to peeing when we sneeze – find out how the right advice from a physiotherapist could change your life.
‘Are you doing your Kegel exercises?’ It’s a question we often hear when it comes to problems with the waterworks, but is it the right question?
Women’s health physiotherapist Fiona Mitchell has been working with women (and men) with pelvic floor concerns for many years and she says there is no ‘one size fits all’ to improving its function. And, we shouldn’t be looking at it in isolation – it is affected by stress, trauma, muscle imbalances and tension and even the position of our feet.
Q. What is the pelvic floor and how does pregnancy, childbirth and menopause affect it?
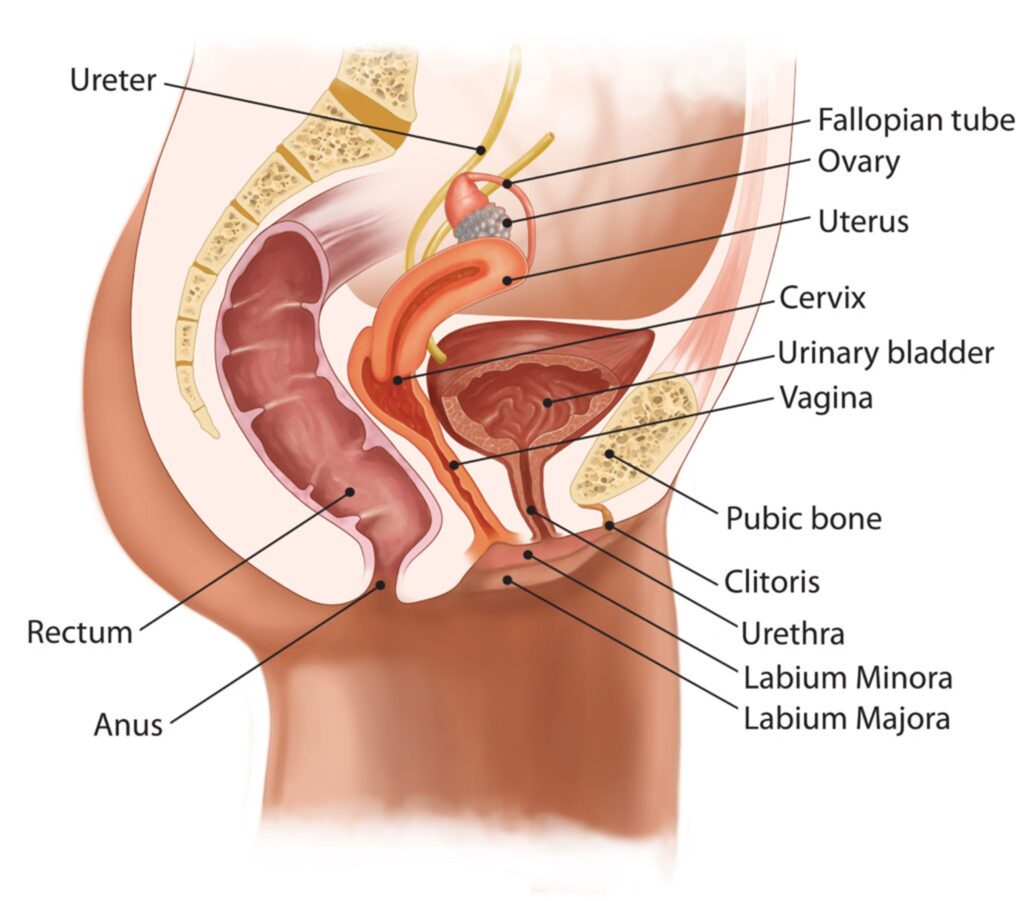
The pelvic floor is a combination of muscles, tendons ligaments that help support our internal organs including the vagina, bladder and rectum. But it’s not just a sling of muscles, it’s also how these muscles attach to the hips and surrounding bones towards the back and, it’s affected by other muscles in the body that can affect the angle of the hips, including our thigh muscles, abdominal and back muscles.
The weight of carrying a baby can affect it as can childbirth and, our hormones. Other things like constipation can also be an issue.
Post caesarean births – with 9 layers of scar tissue, affect the pelvic floor too, as can other scars like episiotomy scars. “This is a huge part of what we deal with”, says
And when it comes to hormones, “postnatally the decline in oestrogen can create symptoms of vaginal dryness that leads to painful sex, and the episiotomy and C-sections scars don’t heal as well as you’d like”, she says.
And with perimenopause, “it can just sneak up on you. You might find that you aren’t as well lubricated as before or that you’re having increased cases of UTIs or thrush, and if you’ve had surgery or an episiotomy that might start to play up.”
But ones of the most common things she sees is stress or urge incontinence and, frequency issues.
“It’s those kind of oops moments, that we see. You might cough, sneeze or jump and pee or may think that you have to make sure that your bladder is empty before you exercise. Some women have it when they laugh. The stress incontinence can also be caused by an over-acitve or hypertonic pelvic floor”, she says.
So what do we do?
Mitchell says we need to ensure we are breathing properly first.
Your diaphragm sits under the lungs and we have a lovely motion between it and the pelvic floor – so if you’re doing pelvic floor exercises you need to be exhaling. Start by tightening around the anal passage first and as you work from back to front.

How to do the Kegel’s properly
There is a NHS recommended app called the Squeezy app that tells you how to contract and relax, she says.
And she says there are two different types of muscle we need to be working – the fast and slow twitch muscle fibres – se we need to do sone long, slow and hold clenches, and some quick ones. Start off slowly, and if you’re finding it difficult you can even start when you’re lying down, she says.
Then, move to sitting or standing. “Ideally we want to get you doing these when you’re standing up, because that’s when you’re going to experience the leakage.”
But it’s not just the pelvic floor you need to think about.
“We know that by moving the lumbar spine that affects the pelvic floor and we know that moving the hips affects the pelvic floor, so we need to integrate those muscles too. So we need to think about shoulder exercises, or squats or moving against resistance. It could be a ball between the knees or band resistance above the knees. If you can work of other areas that affect the pelvic floor that’s a good thing to do.”
“Everything is connected. We often find that people who have pelvic floor pain are tooth clenchers or have neck pain- so sometimes we’ll recommend exercises for the neck or jaw. But then on the other end, the position of the feet can make a difference to the pelvic floor. It’s not just looking at the pelvic floor – it’s looking head to toe really,” she says.
Q. Can devices help?
There are a lot of things on the market, Mitchell says, but it’s important to know what it is you’re using and why.
If you’re using weights like they should be properly designed with a medical grade silicone or metal – not a porous stone.
But, they aren’t suitable for everyone.
“It could be that your pelvic floor is over active, that you’re not breathing properly – so you may not need to invest in anything. If you do, always look for something that’s been recommended by a physiotherapist.”
“When it comes to overactive pelvic floors women will often have back pain or pain with sex. They may have an underlying issue like endometriosis or have suffered some form or trauma or abuse, and they’ve created a protective spasm. We’ve got to start realising that the pelvic floor is like the muscles in the rest of our body, we can hold the same tension through our pelvic floor as we do in our neck or shoulders”, she says. “So stress has a massive effect- we can hold that in our pelvic floor too.”
And this all seems to come to a head around menopause, she says.
Breathing, low wide breaths are important. “We want to calm everything down, we want to switch off and bring ourselves into a rested state. As we breathe better we relax and our abdominals, our core and our shoulders – and our pelvic floor.”
Q. Does being overweight make things worse?
Yes, unfortunately. “If your belly is drawing you forward, it’s going to have an effect on the pelvic floor. And it’s going to put extra pressure on your pelvic floor and increase the risk of leakage and prolapses.
Prolapses
There are four main types:
Cystocele or anterior- when the bladder pushes backwards into the vaginal wall
Rectocele or posterior- when your rectum pushes forwards into the vaginal wall
Uterine – where your cervix or uterus comes down
Urethrocele – where the urethra dips backwards into the vaginal wall.
There is also the vagina vault prolapse that can happen after a hysterectomy.
These are graded 1-4. Grade 1 you may not notice, grade 2, you may start to see symptoms, grade 3 – you can see the prolapse, grade 4- its protruding.
Physiotherapy is recommended for grades 1-2 and can help with grades 3 and 4 – and it can help prepare you for surgery and afterwards.
Vaginal oestrogen can help if you’re perimenopausal, menopausal or post delivery. “Our vulva and pelvic floor, including our bladder and the end of our urethra are very dependant on oestrogen. The end of the urethra may become more prominent and that can increase the risk of UTI’s. But the vaginal oestrogen can really make a difference to bladder issues and incontinence, it really does change lives. It can increase the plumpness of the tissue it can really improve a number of conditions”, she says.
Once you start using it, you need to keep using it, she warns. “Once that oestrogen has decreased in that area, it’s not going to make a miraculous recovery and come back.”
But it’s not just all about declining oestrogen, childbirth or being overweight.
Talking pooh
“The biggest driver of prolapses is constipation”, according to Mitchell.
As our oestrogen levels drop our digestive system changes as we may be more prone to constipation, and this puts pressure on the pelvic floor too. It can be a contributing factor to stress and urge incontinence and can make the symptoms of prolapse worse as it’s push down on the pelvic floor.
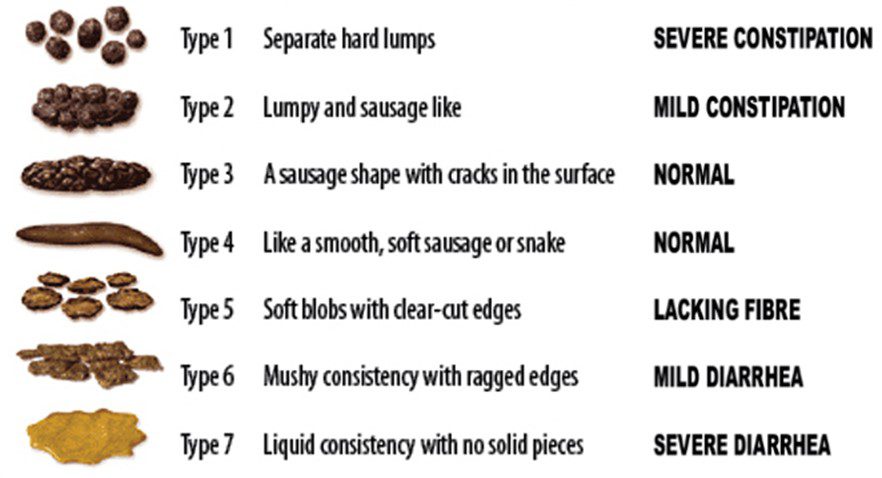
The Bristol Pooh Chart
“To have the optimal stool, we need to be well hydrated, be eating enough fibre, exercising, and our bowels really love rotation. If you’re stiff in the upper back, that’ll have an effect on your digestive system. Massage of the stomach can also help the whole passage of waste.”
“If you find that you’re straining you need to do something about it”, https://blog.harleystreetemporium.com/wp-content/uploads/2017/01/pool-floatie-e1483467263498.jpg says.
Drinking more water, adding more fibre to your diet, drinking less tea, coffee and alcohol and eating more fibre in cereals like oats and grains, fruit, nuts and veggies are a good place to start.
The Squatty potty
Using a foot stool or something that you can put your feet up on can make a huge difference to the passage of waste. If your knees are raised above your hip height it puts the rectum at a better angle for passing the pooh out. “We weren;’t designed to sit on a toilet, so when you bring your knees up your rectum is straight, and you don;t have to push the pooh around an angle.”
This is a simple way of avoiding straining, and if we breath well, even a ‘mooing’ sound can’t help. “the most important thing is that we don’t repetitively strain.
Drink a litre and a half to two litres a day – of water – not alcohol, coffee or tea, and try not to strain. Herbal teas are ok – but remember green tea is caffeinated. Flax seeds are also good and it’s high in fibres, omega 3 and phytoestrogens. Pumpkin seeds are great too, she says.
If you’re feeling like you need to go all the time, caffeinated drinks can make that worse.
Q. Feeling like you haven’t finished?
There are devices that you can put in your vagina that help apply pressure to the rectum and help ease the pooh out – or, she says, you can even use your thumb. You don’t have to press hard, but a gently support through the posterior wall.
Q. Do you need to stop exercising?
Mitchell says you don’t need to stop unless you’re feeling uncomfortable. There are pessaries that can be inserted when exercising that can help stop leakage and a rehabilitation program can help to reduce the need for those. And, keep it low impact until you’re sorted.

