Sexual dysfunction

You may not have heard about it but female sexual dysfunction is one of the biggest unspoken issues affecting female health and wellbeing. Dija Ayodele investigates what it is and what you can do about it.
Are you less interested in sex? Taking longer to get in the mood? Perhaps sex is great but you find yourself sore and in pain during or afterwards? Do you feel an itchy burning sensation in your vagina or the skin around it (which may be flaky or looking less than a vibrant pink)? If you’re nodding yes to any or all of these questions, then you may have what’s known as Female Sexual Dysfunction or FSD.
FSD is a catch all term for a number of symptoms that affect female sexual health ranging from low libido, difficulty getting aroused, inability to achieve orgasm (even after lengthy stimulation) and pain during sexual intercourse. Women often experience more than one of these complaints together.
Uncovering FSD
It is very difficult to get an exact number, however, anecdotally FSD affects 40-60% of the female population at some stage in life. It can be a very isolating and frustrating condition – one that’s been swept under the carpet for many years.
“Female sexual dysfunction is a huge problem in the UK,” according to Dr Shirin Lakhani, a GP and also the owner of Elite Aesthetics in Kent, but says that is not really acknowledged. “It’s not a condition recognised by the NHS. Even though there are many physical symptoms, it is treated as a psychological issue.”
It tends to strike at various key life stages – predominantly around childbirth and menopause.“There is a large body of evidence that shows FSD tends to occur mainly during periods of hormonal upheaval,” Dr Lakhani says.

Pregnancy and FSD
Pregnancy, post-pregnancy and while breastfeeding are common times for women to experience FSD. Although it may be transient, the demands that pregnancy and subsequently a new baby can put on the body can see sexual desire plummet to an understandably low level.
“Childbirth trauma can be a major driver for FSD,” adds Dr Lakhani.
Menopause and FSD
In varying degrees FSD affects both perimenopausal and menopausal women. Menopause lowers oestrogen levels in the body. The face is often the focus of attention when women hit menopause as the lack of oestrogen seemingly speeds up the aging process. But it’s not just the face that’s affected – other parts of the body also suffer from lower oestrogen levels too.
Your breasts, vagina and labia all have oestrogen receptors and the lower oestrogen levels results in thinner vaginal walls, lack of lubrication and loss of skin elasticity.
Dr Louise Newson, GP and Menopause expert says “7 out of 10 women going through the menopause can experience symptoms including vaginal dryness, irritation and pain. Some women even find sitting down uncomfortable.”
And she says they often suffer in silence.
“Many women are not receiving treatment and are not talking about their symptoms.”
Health and FSD
Psychological issues, if left untreated, also play a role in FSD. Anxiety, depression, emotional conflicts, stress, previous or current sexual abuse are all contributory factors that reduce sexual responsiveness and performance. Likewise, major illnesses can also throw the body and hormones into disarray. Cancer (and treatments such as chemotherapy), diabetes and heart problems all play a role when considering the causes of FSD.
Medications
Routine prescribed medications can also bring on the symptoms of Female Sexual Dysfunction at any age. For example, some prescribed antidepressants, antihistamines and blood pressure medications can lower libido and also affect your ability to achieve orgasm.

What can be done about it? Available Treatments
Like the causes, treatments for FSD are broad but can be split into two main camps – medical and non medical.
With the latter, one of the most simple solutions is Talking Therapy (i.e. Cognitive Behavioral Therapy), especially if the origin is psychological. According to Dr. Lakhani, “the NHS tends to refer women for psychosexual treatment.”
There are counselors who specialize in sex and relationship problems and can provide education on processing and enhancing your body’s sexual responses.
Another inexpensive solution is the use of lubricants e.g. KY Jelly to make sexual intercourse more comfortable and help with vaginal dryness. If you couple this with a device like a vibrator for clitoral stimulation you also stimulate arousal that may lead to improvements in your sex life.
Hormones
The medical approach to treating FSD will first address any underlying medical conditions or hormonal imbalance. If there is a hormonal basis, doctors will recommend hormonal therapy first to redress the balance.
Dr Daniel Sister, hormone specialist and creator of the Dracula Therapy, recommends ruling out any underlying medical issues before local vaginal treatments are administered. “Hormonal testing is a must, as most of the time there is a hormonal deficiency, especially in the older patient.”

One hormone that may be deficient is, perhaps surprisingly, testosterone. Although primarily a male hormone, a small amount of testosterone is necessary for female sexual health. Dr. Newson is an advocate for low doses of testosterone.
“When women’s levels of testosterone decreases, women may find that they desire sex less often and when they do have sex, it is not as pleasurable as it used to be. Testosterone is really beneficial at improving general well-being, mood, energy, concentration and also sex drive or libido.”
Applying localised oestrogen through a vaginal ring, cream, pessary or tablet is a common prescription that improves vaginal tone and delivers improved vascular function through increased blood flow.
Vaginal rejuventation
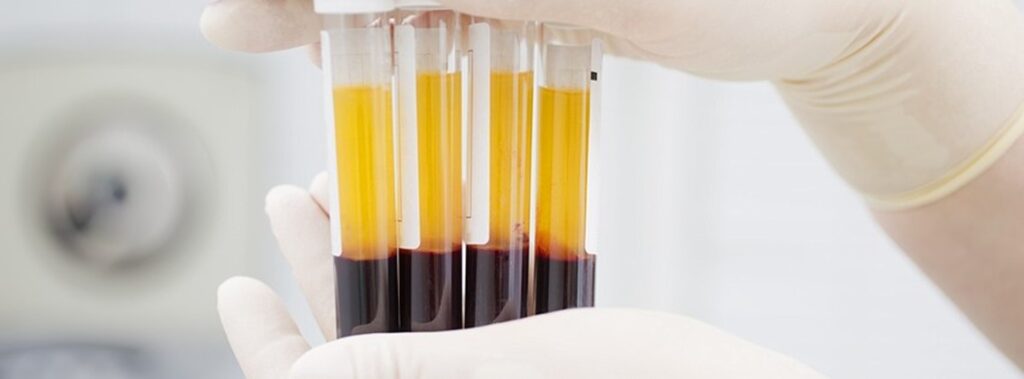
At Dr Sister’s practice, addressing hormonal issues often brings about an improvement in symptoms. However, sometimes a more invasive treatment is required. Hence, alongside clinical nurse specialist Claudia McGloin, Dr. Sister developed the Revulva technique – a form of treatment with PRP (Platelet Rich Plasma) that involves drawing blood, spinning it down to get the platelet rich plasma and re-injecting an enhanced version to rejuvenate vaginal tissue.
“Revulva uses your entire blood plasma that has been enhanced with other beneficial ingredients e.g. hyaluronic acid injected into vaginal tissue to stimulate the area’s own natural sensations and enhance sexual wellbeing.”
Dr Sister advocates tailoring the best treatment(s) to the individual patient’ needs when addressing FSD. He says “second level solutions also need to be considered as sometimes plasma injections wouldn’t be enough, a combination treatment would be required combining hormones, plasma and technological devices.”
Another relatively new treatment gaining popularity is the O Shot, which Dr. Lakhani also administers.
It involves injecting plasma into well numbed vaginal tissue and the clitoris. (As painful as that sounds the area is numbed first!) Since she started the treatments in 2015, Dr Lakhani has seen steady interest and has administered over 200 O Shot injections.
“It’s starting to become a popular treatment as awareness increases and women recognize that there are treatments for sexual dysfunction available. Radio Frequency (to address vaginal laxity) and the O Shot together give phenomenal results,” she says.
Interestingly the O Shot and Revulva treatments are also popular and successful treatments for stress incontinence.
Dr Lakhani says the majority of people who come for the procedure are there to improve their sex lives, but emphasizes that relieving stress incontinence “is one of the main reasons people seek out the O Shot.”
Although relatively new, and in spite of the need for a larger body of practical evidence for plasma based FSD treatments, the results to date appear to be very promising for the symptoms of FSD and stress incontinence.
Also new on the market is a 30 minute treatment called Geneveve. Using a handheld radio frequency which cools and heats vaginal tissue, new collagen production is stimulated (which helps fortify the vaginal walls). It is currently being distributed in the UK. Whilst it is difficult to say exactly how effective it is on the market, findings from two clinical studies indicated that 90% of women on the trial still had increased and sustained tightening and sensation 12 months post treatment.
Dr Lana Tattum, from the london aesthetics clinic ‘Ideal U’ has been providing the Geneveve treatment for about a year and says there are a number of advantages to the treatment ranging from the time it takes to a few other unexpected benefits.
“Ittakes just 30 minutes and has no down time, meaning many women can resume normal activities straight after. The treatment itself uses tiny pulses of radiofrequency energy to gently heat the deeper layers of the vaginal tissue whilst simultaneously cooling and protecting the delicate surface. After the treatment and over the next 3 months, the body responds by developing healthy, new collagen and elastin so the vaginal tissue is revitalised and sexual sensation is restored.
“We are also finding that many of our patients are seeing a huge improvement in their urinary incontinence issues which is an added benefit to the treatment.”
Price is determined by the clinic but is typically about £2500.
To sum up:
If you think you might have Female Sexual Dysfunction there are more options than ever for treatment and to improve the quality of your health. Speak with your doctor about which treatments might be the best match for your needs.

